IN THIS UPDATE:
- Factors That Predict Walking Difficulty In Elderly
- Low Vitamin D Levels Linked To Depression
- Age-Related Blindness May Be Warded Off By Grapes
- 45 Could Mark The Onset Of Cognitive Decline
- Alzheimer’s Patients Benefit From Light Therapy
1. Factors That Predict Walking Difficulty In Elderly
 Yale School of Medicine researchers have found that the likelihood of becoming disabled with age increases with the following factors: having a chronic condition or cognitive impairment; low physical activity; slower gross motor coordination; having poor lower-extremity function; and being hospitalized. Women are also more likely than men to become disabled in their later years.
Yale School of Medicine researchers have found that the likelihood of becoming disabled with age increases with the following factors: having a chronic condition or cognitive impairment; low physical activity; slower gross motor coordination; having poor lower-extremity function; and being hospitalized. Women are also more likely than men to become disabled in their later years.
Based on 12 years of data, the findings are published in the Jan.17 issue of Annals of Internal Medicine by a research team led by Thomas Gill, M.D., the Humana Foundation Professor of Geriatric Medicine and professor of medicine, epidemiology, and public health at Yale School of Medicine.
With age, many people can no longer walk short distances or drive a car, and those with long-term loss of mobility have difficulty regaining independence.
“Losing the ability to walk independently not only leads to a poorer overall quality of life, but prolonged disability leads to higher rates of illness, death, depression and social isolation,” said Gill, who followed a group of 641 people aged 70 or older who could walk a quarter mile unassisted or who were active drivers at the start of the study. All participants could perform essential activities of daily living, such as bathing and dressing.
Gill and his team assessed the participants for changes in potential disability risk factors every 18 months between 1998 and 2008. They also assessed the participants’ mobility each month. Those who said they needed help from another person to walk a quarter mile were considered to be walking disabled. Those who said that they had not driven a car during the past month were considered driving disabled.
On a monthly basis, the research team also assessed the participants’ exposure to potential causes of disability, including illnesses or injuries leading to hospitalization and restricted activity, which increased the likelihood of long-term disability by 6-fold.
The team found that multiple risk factors, together with subsequent illness and injury leading to hospitalization and restricted activity, are associated with an increased likelihood of developing long-term walking and driving disability. The team considered a disability to be long term if it persisted for at least six months.
“We’ve learned that targeted strategies are needed to prevent disability among older people living independently in the community,” said Gill.
Source: Yale School of Medicine, January 17, 2012
2. Low Vitamin D Levels Linked To Depression
 New research has looked at whether social media could be used to track an event or phenomenon, such as flu outbreaks and rainfall rates.
New research has looked at whether social media could be used to track an event or phenomenon, such as flu outbreaks and rainfall rates.
Low levels of vitamin D have been linked to depression, according to UT Southwestern Medical Center psychiatrists working with the Cooper Center Longitudinal Study. It is believed to be the largest such investigation ever undertaken.
Low levels of vitamin D already are associated with a cavalcade of health woes from cardiovascular diseases to neurological ailments. This new study – published in Mayo Clinic Proceedings – helps clarify a debate that erupted after smaller studies produced conflicting results about the relationship between vitamin D and depression. Major depressive disorder affects nearly one in 10 adults in the U.S.
“Our findings suggest that screening for vitamin D levels in depressed patients – and perhaps screening for depression in people with low vitamin D levels – might be useful,” said Dr. E. Sherwood Brown, professor of psychiatry and senior author of the study, done in conjunction with The Cooper Institute in Dallas. “But we don’t have enough information yet to recommend going out and taking supplements.”
UT Southwestern researchers examined the results of almost 12,600 participants from late 2006 to late 2010. Dr. Brown and colleagues from The Cooper Institute found that higher vitamin D levels were associated with a significantly decreased risk of current depression, particularly among people with a prior history of depression. Low vitamin D levels were associated with depressive symptoms, particularly those with a history of depression, so primary care patients with a history of depression may be an important target for assessing vitamin D levels. The study did not address whether increasing vitamin D levels reduced depressive symptoms.
The scientists have not determined the exact relationship – whether low vitamin D contributes to symptoms of depression, whether depression itself contributes to lower vitamin D levels, or chemically how that happens. But vitamin D may affect neurotransmitters, inflammatory markers and other factors, which could help explain the relationship with depression, said Dr. Brown, who leads the psychoneuroendocrine research program at UT Southwestern.
Vitamin D levels are now commonly tested during routine physical exams, and they already are accepted as risk factors for a number of other medical problems: autoimmune diseases; heart and vascular disease; infectious diseases; osteoporosis; obesity; diabetes; certain cancers; and neurological disorders such as Alzheimer’s and Parkinson’s diseases, multiple sclerosis, and general cognitive decline.
Investigators used information gathered by the institute, which has 40 years of data on runners and other fit volunteers. UT Southwestern has a partnership with the institute, a preventive medicine research and educational nonprofit located at the Cooper Aerobics Center, to develop a joint scientific medical research program aimed at improving health and preventing a wide range of chronic diseases. The institute maintains one of the world’s most extensive databases – known as the Cooper Center Longitudinal Study – that includes detailed information from more than 250,000 clinic visits that has been collected since Dr. Kenneth Cooper founded the institute and clinic in 1970.
Other researchers involved in the study were Dr. Myron F. Weiner, professor of psychiatry and neurology and neurotherapeutics; Dr. David S. Leonard, assistant professor of clinical sciences; lead author MinhTu T. Hoang, student research fellow; Dr. Laura F. DeFina, medical director of research at The Cooper Institute; and Benjamin L. Willis, epidemiologist at the institute.
Source: UT Southwestern Medical Center, January 7, 2012
3. Age-Related Blindness May Be Warded Off By Grapes
 Can eating grapes slow or help prevent the onset of age-related macular degeneration (AMD), a debilitating condition affecting millions of elderly people worldwide? Results from a new study published in Free Radical Biology and Medicine suggest this might be the case. The antioxidant actions of grapes are believed to be responsible for these protective effects.
Can eating grapes slow or help prevent the onset of age-related macular degeneration (AMD), a debilitating condition affecting millions of elderly people worldwide? Results from a new study published in Free Radical Biology and Medicine suggest this might be the case. The antioxidant actions of grapes are believed to be responsible for these protective effects.
The study compared the impact of an antioxidant-rich diet on vision using mice prone to developing retinal damage in old age in much the same way as humans do. Mice either received a grape-enriched diet, a diet with added lutein, or a normal diet.
The result? Grapes proved to offer dramatic protection: the grape-enriched diet protected against oxidative damage of the retina and prevented blindness in those mice consuming grapes. While lutein was also effective, grapes were found to offer significantly more protection.
“The protective effect of the grapes in this study was remarkable, offering a benefit for vision at old age even if grapes were consumed only at young age,” said principal investigator Silvia Finnemann, PhD, Department of Biological Sciences, Fordham University in New York.
Dr. Finnemann noted that results from her study suggest that age-related vision loss is a result of cumulative, oxidative damage over time. “A lifelong diet enriched in natural antioxidants, such as those in grapes, appears to be directly beneficial for RPE and retinal health and function.”
Age-related macular degeneration is a progressive eye condition, leading to the deterioration of the center of the retina, called the macula. It is the leading cause of blindness in the elderly. Aging of the retina is associated with increased levels of oxidative damage, and oxidative stress is thought to play a pivotal role in the development of AMD.
In AMD, there is a known decline in the function of retinal pigment epithelium cells (RPE), which are the support cells for the photoreceptors in the retina that are critical to the process of converting light into sight. The RPE dysfunction is caused by 1) a build-up of metabolic waste products (known as lipofuscin) in the RPE itself and 2) an oxidation burden on the RPE that compromise important metabolic pathways. The resulting dysfunction, distress and often death of the RPE cells leads to AMD.
This study showed that adding grapes to the diet prevented blindness in mice by significantly decreasing the build-up of lipofuscin and preventing the oxidative damage to the RPE, thus ensuring optimal functioning of this critical part of the retina.
“Preserving eye health is a key concern as we age and this study shows that grapes may play a critical role in achieving this,” said Kathleen Nave, president of the California Table Grape Commission. “This is good news for consumers of all ages who enjoy grapes, and adds to the growing body of evidence that grapes offer an array of health benefits.”
Source: Fordham University, January 13, 2012
4. 45 Could Mark The Onset Of Cognitive Decline
 Increased life expectancy implies fundamental changes in the composition of populations, with a significant rise in the number of elderly people. These changes are likely to have a massive influence on the life of individuals and on society in general. Abundant evidence has clearly established an inverse association between age and cognitive performance, but the age at which cognitive decline begins is much debated. Recent studies concluded that there was little evidence of cognitive decline before the age of 60.
Increased life expectancy implies fundamental changes in the composition of populations, with a significant rise in the number of elderly people. These changes are likely to have a massive influence on the life of individuals and on society in general. Abundant evidence has clearly established an inverse association between age and cognitive performance, but the age at which cognitive decline begins is much debated. Recent studies concluded that there was little evidence of cognitive decline before the age of 60.
However, clinical studies demonstrate a correlation between the presence of amyloid plaques in the brain and the severity of cognitive decline. It would seem that these amyloid plaques are found in the brains of young adults.
Few assessments of the effect of age on cognitive decline use data that spans over several years. This was the specific objective of the study led by researchers from Inserm and the University College London.
As part of the Whitehall II cohort study, medical data was extracted for 5,198 men and 2,192 women, aged between 45 and 70 at the beginning of the study, monitored over a 10-year period. The cognitive functions of the participants were evaluated three times over this time. Individual tests were used to assess memory, vocabulary, reasoning and verbal fluency.
The results show that cognitive performance (apart from the vocabulary tests) declines with age and more rapidly so as the individual’s age increases. The decline is significant in each age group.
For example, during the period studied, reasoning scores decreased by 3.6 % for men aged between 45 and 49, and 9.6 % for those aged between 65 and 70. The corresponding figures for women stood at 3.6% and 7.4% respectively.
The authors underline that evidence pointing to cognitive decline before the age of 60 has significant consequences.
“Determining the age at which cognitive decline begins is important since behavioural or pharmacological interventions designed to change cognitive aging trajectories are likely to be more effective if they are applied from the onset of decline.” underlines Archana Singh-Manoux.
“As life expectancy continues to increase, understanding the correlation between cognitive decline and age is one of the challenges of the 21st Century” she adds.
Source: Whitehall II Cohort Study, January 11, 2012
5. Alzheimer’s Patients Benefit From Light Therapy
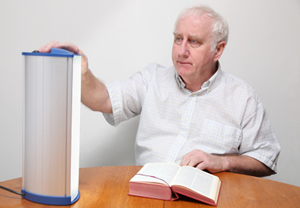 Exposure to light appears to have therapeutic effects on Alzheimer’s disease patients, a Wayne State University researcher has found.
Exposure to light appears to have therapeutic effects on Alzheimer’s disease patients, a Wayne State University researcher has found.
In a study published recently in the Western Journal of Nursing Research, LuAnn Nowak Etcher, Ph.D., assistant professor of nursing, reported that patients treated with blue-green light were perceived by their caregivers as having improved global functioning.
Caregivers said patients receiving the treatment seemed more awake and alert, were more verbally competent and showed improved recognition, recollection and motor coordination. They also said patients seemed to recapture their personalities and were more engaged with their environment. Patients’ moods also were described as improved.
Etcher’s work is inspired by her interest in a phenomenon known as “sundowning,” when Alzheimer’s patients sleep during the day, wake up later and may be up all night long. Part of her doctoral research was to utilize light, a common intervention for circadian disorders, to regulate the rest-activity patterns of women with Alzheimer’s.
This study, Etcher said, was an effort to address disagreement among researchers on the effect of therapeutic light in regulating rest-activity patterns in Alzheimer’s patients. The study involved 20 women older than age 65 with Alzheimer’s dementia from nursing homes in southeast Michigan. Each patient was assigned randomly to an experimental group receiving blue-green light treatments or a control group receiving dim red light.
A commercially available visor used to treat seasonal affective disorder and jet lag was used to administer the light to patients. Caregivers – patients’ family members and nursing facility personnel – were not told which type of light was hypothesized to have physiologic effects.
Although blue-green light recipients comprised the active experimental group, Etcher said she was surprised when some recipients of red light – the placebo group – also were reported as showing improvements, with caregivers saying their patients were calmer and had reduced resistance to care.
The level of effects varied, Etcher said, noting that while the blue-green group recipients were largely reported by caregivers as showing improvement, a few showed little to no effect from the treatments.
“Some of the rest-activity pattern disruptions that we see associated with Alzheimer’s dementia may not necessarily be circadian based,” Etcher said. “They may be due to unmet needs, pain or other phenomena, and therefore would not respond to an intervention aimed at regulation of the circadian system.”
Calling her study preliminary, she said it now needs to be replicated with a larger sample and different demographics.
In addition to ascertaining which behaviors are circadian based, establishing which methods are most appropriate to analyze data like Etcher’s requires exploration, she said. She is proposing further work that uses two different nonlinear analytic methods to examine sensitivity and specificity to detect change in circadian patterns, with a long-term goal of developing interventions to regulate those patterns to the benefit of patients’ overall function.
“If they sleep better at night, and are more awake during the day, they can eat, they can interact with other people and they can take advantage of other cueing agents in the environment,” she said. “In addition to light during daytime and darkness during the nighttime, smells at mealtimes, food intake, interactions – all these things in conjunction help regulate our day.”
Source: Wayne State University, January 13, 2012
If you have written or find any articles that you would like to contribute to the Warman E-Update, please contact Brenda Head at bhead@warmanhomecare.com or by telephone at (877) 694-4264. If any of your colleagues are not receiving the Warman E-Update, please send his or her e-mail address to bhead@warmanhomecare.com for inclusion.
Call us at (888)-243-6602 to discuss how we can help keep your loved one safe and happy at home.

